Thought Leadership
Making a Difference: How Policy and Advocacy Changes Lives for Patients and Their Communities
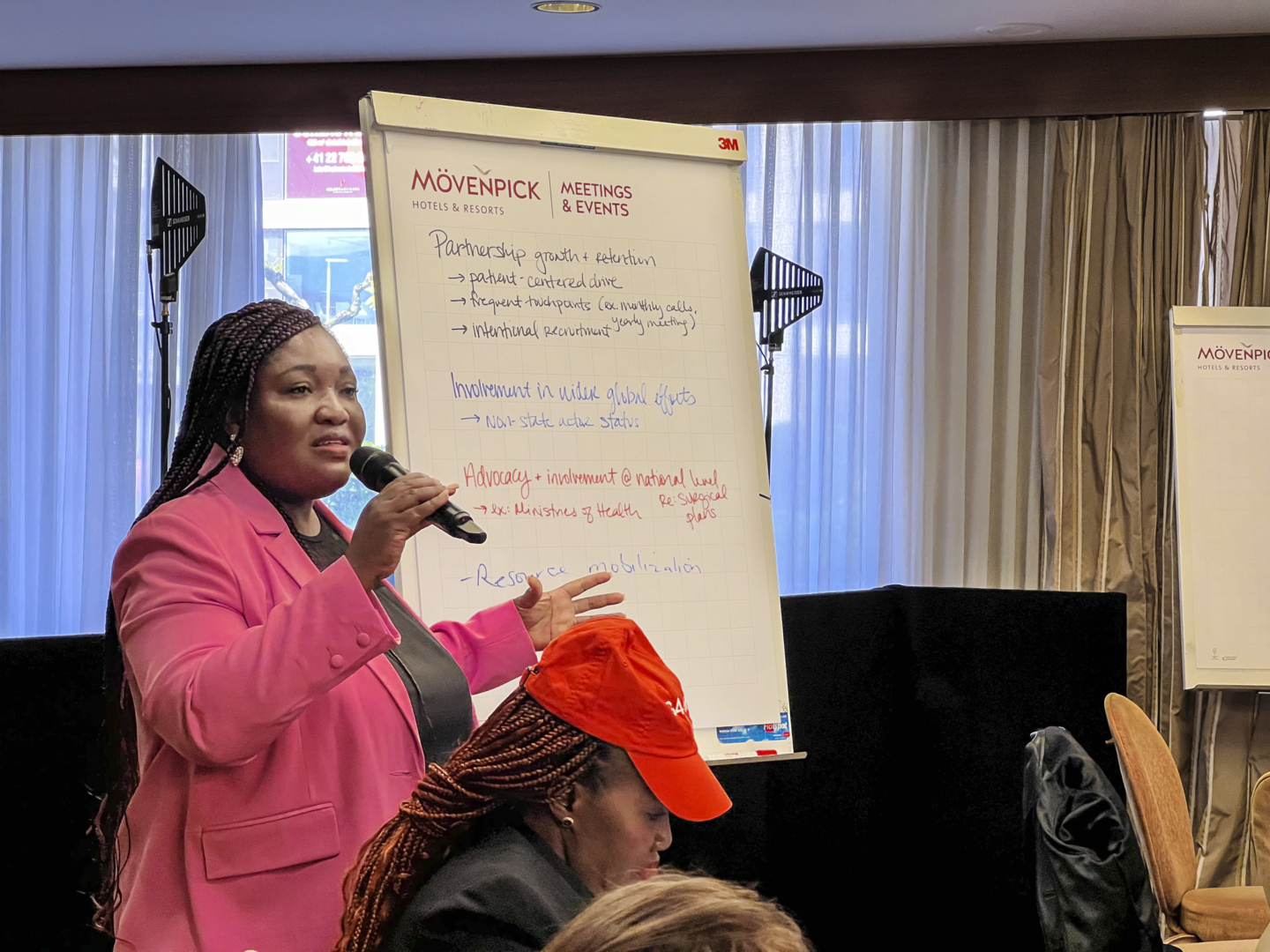
Operation Smile’s Irene Dzirasa explains how she and her colleagues work with governments and global partners to ensure better, safer surgeries throughout Africa and the world.

Picturing policy and advocacy work leads to images of big conference rooms, complex data and well-researched presentations. While that is a part of what Irene Dzirasa and her teammates do for Operation Smile, there is also a great deal of local, onsite health policy research that can help transform communities.
“We go into the field to specific hospitals to collect data. For example, if a hospital reports that they have two anesthesia machines, we go to the hospital to verify whether or not they are functioning,” explains Dzirasa, who serves as regional lead in Africa to the policy and advocacy department at Operation Smile. “These visits help ensure that national health data reflects the actual conditions on the ground. And then we use that updated data to inform national planning, prioritize investments and advocate for targeted interventions that directly address the needs of frontline providers and patients.”
Working with both caregivers and patient advocates, Dzirasa finds ways to strengthen surgical care, not only for patients with cleft conditions, but for anyone being treated at local hospitals in the region. Some of her work has included representing Operation Smile at the Global Alliance for Surgery Obstetric Trauma and Anesthesia (G4 Alliance). She also serves as the chairperson of the African working group of the G4 Alliance, to prioritize of surgery, obstetric, trauma and anesthesia (SOTA) care in national health agendas across the African continent.

We spoke with Dzirasa about her role at Operation Smile and how policy and advocacy work is a crucial part of the nonprofit’s goals to make a lasting impact by expanding access to safe, timely and affordable health care around the world.
Tell us about your career journey. How did you come to work with Operation Smile?
Irene Dzirasa: Prior to joining Operation Smile, I worked with the Ghana Health Service as a public health nutritionist. Then I went to study for my master’s degree in international public health at the Liverpool School of Tropical Medicine. With a background in nutrition, I developed an interest in infant and young child feeding, and I learned that having a cleft condition can greatly affect a baby’s ability to latch on during breastfeeding or even swallowing may be a problem. So, I focused my dissertation on cleft care. I joined Operation Smile in 2022 directly from my master’s program.
As the regional lead for policy and advocacy, what are your goals? What kind of work do you do?
ID: In my role, I work closely with Operation Smile’s country offices — with a strong focus on Africa — to develop policy and advocacy strategies that are both locally grounded and nationally aligned. Each strategy ensures that the country office’s goals are not only in sync with national health priorities but also contribute to shaping them.
We do this by working with ministries of health, national surgical planning teams, NGOs, and development partners to find shared priorities and bridge the gaps.
We also do work in the field, such as verifying surgical infrastructure and engaging with local care teams. Our goal is to become active contributors in the development and implementation of sustainable, equitable health policies that everyone in the communities can benefit from — particularly in surgical and anesthesia care
Why is a focus on surgical care policy important?
ID: Surgical care was once considered a neglected aspect of global health because most conversations within global health communities were centered around HIV, malaria and tuberculosis. Of course, these are serious diseases, and they affect many people. But the number of lives lost due to the lack of access to surgery, obstetric, trauma and anesthesia (SOTA) care is even higher.
In my current role, I also look at which African countries have developed national surgical plans and do not have the funds they need to make these plans a reality. I work with governments, ministries of health and strategic partners to identify sustainable funding for implementation of national surgical plans and to improve overall access to SOTA care. The goal is to make surgery and care more accessible, strengthen local health systems and have a lasting impact on communities.

Is there an initiative you’ve worked on that demonstrates the positive effect of focusing on surgical care?
ID: One of the most recent milestones has been working with the government of Ghana and the Ministry of Health to develop Ghana’s very first national surgical, obstetric and anesthesia plan. As part of the development of this plan, we did a baseline survey to look at the current state of surgery, obstetrics, trauma and anesthesia care. We went into the field to specific hospitals to collect data. During this process, the surgical care teams were very excited to see a team from the Ministry of Health plus Operation Smile coming to visit them to discuss what challenges they have.
This plan is an important step for Ghana and can also be a guide for other countries in Africa as they work to improve surgical care in their own health systems.

We looked at all the areas that impact surgical care, even the electricity. We wanted to know if the lights went off did they have a standby generator? Does the power switch automatically to the standby generator or does someone need to go and fix it in. If there is someone having surgery when it is being fixed, what is happening to the person?
Are you seeing how your work impacts not only the hospitals but helps build the trust and confidence of the patients and their families?
ID: The public realizes that the particular care they are receiving is getting the needed attention. They know there is someone who goes to check on the equipment, and it is being serviced and sterilized. It builds trust in their system.
What are patient advocates, and why are they important?
ID: These are former surgical patients who are now advocating for better access to care. So, it gives them the opportunity to also be part of decision making when it comes to issues around providing the care that is needed. Patients are benefiting directly and are also working directly with us to make it happen.
We also invite patient advocates to speak at some of the high-level meetings that we host, for example the World Health Assembly. When we get them to come and speak at this kind of function, they bring an essential human touch to everything we are discussing around policy.
People have shared their stories about the number of surgeries they required or the number of hours they had to travel before accessing care. At these meetings we have the ministries of health and key decision-makers, and when they hear our patient advocates discussing their surgical journeys, it makes them reflect on their own health systems. Then when they return home, they are eager to make a change.
Operation Smile focuses on expanding access to surgical care starting with cleft conditions. How does strengthening surgical care systems enhance treatment for many kinds of patients?
ID: The work we do with ministries of health, governments and other strategic partners goes beyond cleft care. It touches the entire health system, making it more resilient to deliver any kind of care. For instance, if we support work on a policy which increases the number of anesthesiologists in a particular country, the anesthesiologist is not going to work only on people with cleft conditions. This anesthesiologist is also going to work on people needing abdominal surgery, people coming in for breast surgeries and all other cases. So, it helps make the whole health system more resilient for everyone.
When you think ahead to the next few years, what keeps you hopeful?
ID: One of the key things that keeps me hopeful are the memories of the smiles of children we have provided comprehensive cleft care to. Knowing that the care we provide and the policies that we develop are going to make a lot more families smile keeps me energized.
In the next five years, I hope to see, particularly in areas where I am working, ministries of health and governments having very clear plans to improve surgery and anesthesia care.
Yes, I’m hopeful that many of these policies will be implemented. The momentum is building, and with continued collaboration, we can help these plans become meaningful, sustainable improvements in surgical care.
Learn More about Policy and Advocacy
Want more information about Operation Smile’s work national governments, nonprofit organizations and more?