Our promise of improving health and dignity during the COVID-19 pandemic endures. We're helping front-line health workers stay safe, nourished and empowered to better serve their patients by providing life-saving supplies and equipment, as well as remote training to bolster their response. We’re also providing nutritional assistance, hygiene kits and virtual health services to support people and their health needs so they can thrive. If you can, when you can, help us keep our promise to care for children and create hope for tomorrow.
Now, more than ever it’s our charge to safeguard the health and well-being of individuals around the world. We’re building upon our expertise in delivering cleft surgery and care in resource-limited settings as well as our history of improving the health and dignity of those we serve.
That’s why we’re finding the most meaningful ways that we can support people and their health needs in the communities where we work, even when medical missions are postponed, care centers are closed, and the future feels uncertain. It’s in this uncertainty that our swift action is required, and we’re doing everything that we can to help patients, families, and countries as this affects them.
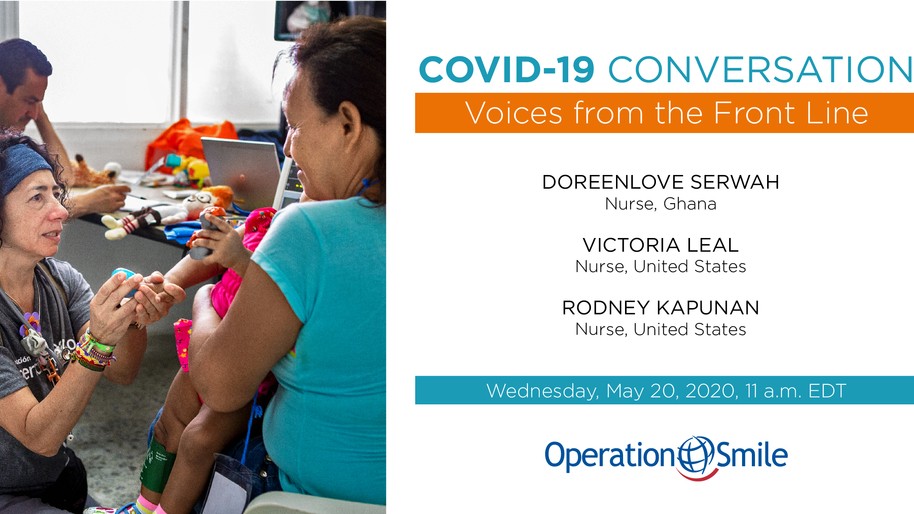
This “COVID-19 Conversation” featured a live question-and-answer session with Operation Smile volunteer nurses Victoria Leal of the United States, Doreenlove Serwah of Ghana and Rodney Kapunan of the United States. The session was hosted by Laura Gonzalez, our digital content manager; and John Streit, our managing editor and writer, moderated the audience’s chat and questions.
Click here to watch our next COVID-19 Conversation.
Event Transcript
Laura: All right. Thanks again, everyone, for joining. My name is Laura Gonzalez, and I am a member of Operation Smile’s storytelling team. We are so excited to introduce the panelists we have here today, but before we do that, I'd like to introduce you to my colleague and co-moderator, John Streit.
John: I'm John Streit, our managing editor and writer. I work really closely with Laura on all of the stories that we present in the COVID-19 Conversation series. We're just super excited to be with our panelists today who represent such a diverse group of people that are out there on the front lines, so thank you guys for joining. Throughout the webinar, I'll be moderating the questions and the chat area, so if you do have any questions that you'd like to ask our panel, we'll have 15 minutes at the end of our conversation where we can address those questions directly to them so we can engage in that.
Enter those directly into the question bar and feel free to use chat function as well. If there is anything I can answer, I'll be providing those answers to you in real time. Yes, just looking forward to the conversation today. Thanks, Laura.
Laura: Thank you. All of these panelists are Operation Smile volunteers, and they are currently serving on the front lines of the COVID-19 pandemic. First up, we have Doreenlove Serwah from Ghana. She joined Operation Smile Ghana as a medical volunteer team as a post-anesthesia care unit nurse in 2016. In addition to becoming an instructor for our American Heart Association life support training, she also became a clinical coordinator, the head nurse in charge of leading the clinical aspect of our medical commissions. In 2018, she was a member of Operation Smile Ghana's first locally conducted medical mission, and today, she is the lead nurse of a pediatric emergency unit at her hospital.
Next, we have Victoria Leal from Florida in the United States. She was born first in Colombia and then moved to the U.S. shortly after graduating from nursing school. She also became an Operation Smile volunteer back in 2011. Since then, she has donated her time, passion, and skill as a pre- and post-operative nurse on 24 of our medical missions around the world. Currently, Victoria is serving in an intensive care unit providing direct care to patients afflicted by COVID-19.
Then last but certainly not least, we have Rodney Kapunan, who's also from Florida in the United States. Rodney is an emergency room nurse originally from the Philippines, currently working in Florida as well. He volunteered on 16 medical missions with Operation Smile serving as an operating room nurse, pre- and post-operative nurse, and most recently as a quality assurance nurse. His wife is also a volunteer for Operation Smile, and the pair bring years of nursing experience to our global family.
Rodney, Doreenlove, Victoria, thank you all so much for joining today.
Doreenlove: Thank you.
Victoria: Thank you
Rodney: Thank you, Laura.
Laura: Of course. We're going to hop right into questions if that's okay with you guys. This first one is for you, Rodney. What does a typical day at work look like during this pandemic, and what's the environment like in the emergency room at your hospital?
Rodney: I just want to make sure that everyone knows the virus is still with us and we still don't have any vaccine or treatment for it. I'm sorry. We're still on heightened alert. Our environment opens up and there's more chances of an outbreak, so we're still doing a lot of personal protection for the patient. We're still limiting our visitors, and we're still trying to isolate a patient that is high probability for COVID to those patients that have no probability. We're trying to not only take care of that patient but also take care of the public as well so that this thing will not come back again.
Laura: Yes, that is so important. Doreenlove, could you speak a little bit about how COVID-19 has affected Ghana?
Doreenlove: Like all other countries, COVID-19 has affected so many areas. In Ghana, we already had a strained health care system, so with this COVID-19, it's strained it more. Now, most of our doctors and nurses who used to work in other areas have been taken to their treatment areas, so they are working there. Then also, patients who have other illnesses are not really getting the needed care because either they are staying at home or they are even afraid to come to the hospitals.
Socially, I think there is something that everybody knows about Ghana, that Ghanaians are touchy people. We hug people, we meet in social settings and all of that. Now, with this social distancing, it's very, very difficult for us because, at times, you forget that you have to keep your distance from one another. You see somebody, and the first instinct is to hug the person or touch the person.
That's one of the ways in which it affected us. We no longer do the things that we used to. Ghanaians are very big on funerals, meetings, ceremonies. Even weekends, extended families come together, I know that, but now, we don't do it. Even religiously, churches are banned. Churches and other religious activities are banned. We are in Ramadan. Muslims are not able to meet to pray together, no church activities. This Easter, I would have had a whole lot of Easter conventions and all of that, but because of COVID-19, we are not able to hold it.
Economically, I think most businesses have come down because buildings are closed, so you cannot import and you cannot export. Also, let's take normal farming, people are not going to farm, so it's even difficult to get the stuffs. Items have either become very scarce or they've become very, very expensive. Yes, so most people have lost their job. Then, when it comes to limitations, I think the limitations run through all the countries: Shortage of PPEs, it's everywhere, but actually, our government is making efforts to resolve that. Then, we had a few treatment centers. When this COVID started, we had a few treatment centers, but as of now, at least for the cases that we have now, we have enough treatment centers to take care of the patients that we have.
Laura: Yeah, we've experienced a lot of the same things that you are mentioning here in the United States. Victoria, do you remember the day that everything changed in your hospital? Could you speak a little bit about what that was like and what you experienced?
Victoria: Yes. I think that it's not just for me; there were big changes in my unit. I think in my personal life, there was a big change. I mean, all the American people, it was a big change that started. I think that I'm never going to forget when that happened. That was just March (13), Friday, that was my overtime. I was normally doing four nights in a row, and that was my fourth night. When I get to work, I saw the people moving around too fast like chaotic environment, ACPs, nurses, secretaries just moving around, try to do assigning, move the patient.
Before they gave us an assignment, we do the huddle. I remember the secretary went to the huddle rooms and start to clean like in a frenetic way, very fast, everything with CaviWipes, and they start to give pieces of information and said, "Hey, you guys, you need to use N95. I think that we are going to have a COVID patient. I have found a scrub for you. Do you need to just use this scrub now? Because I think that we're going to have some admissions tonight." I remember I was surprised. We looked at one another and says, "What is she talking about?" We never hear nothing about COVID in the U.S. We hear news about the coronavirus in China. We never thought that it was going to be among us, ever. We have no clue, no idea it was going to happen.
Then, at that night, one admission came. Old guy, came with shortness of breath, very weak with temperature, was admitted in the negative room. We have two negative pressure rooms in my unit. He was admitted early. That was assigned on just one nurse, the assignment just there for the possible COVID patient that we're going to admit that night. Everybody was starting to feel very anxious like, "Now, I think that it's real. It's real. The virus is here, and they are going to touch us." Then, that night, past midnight, we admit the second patient, an old lady also. Both patients were with very high risk and medical history, very important medical history, but the signs and symptoms are completely the same for both patients. The lab work was very similar … at that point, when they test the patient, the test lasts like five to seven days. We can't wait.
We need to start to treat the patient like COVID even though we don't have any resource. But thanks to God, the daughter of the first patient told us that her father was in contact with somebody who was positive and was in the other hospital. That was very helpful for us because we just know how we're going to be with this patient, how are we going to treat the patient, how are we going to take care of ourselves. That just happened that night.
Then, I came back two days later and was completely different. Completely different. We just started with two patients, and when I came back, my unit was ICU COVID unit, completely. From two patients, we went to 20, 20 … COVID positive, or the symptomatology was exactly. All the patients were the same. Very high oxygen demand.
They start to deteriorate too fast, patient very weak with fever, chills. All the lab work are very similar. My unit was completely sealed. They closed and isolated the unit that when we get there, we say, "What is that? Where are our patients?" We normally used to have ECU patients. Now, everybody was almost ICU patients with high oxygen demands, cannulas, high-flow oxygen, and all the alarms with low oxygen saturation was around the corridors.
Then, when we get there, the A floor is my unit, it's completely isolated, was completely sealed, whoever goes inside can't go outside anymore. Then, they gave us some poppers, a special ventilator. We used it to protect ourselves. Then, we looked like a movie like when you are an astronauts. We just walked through the corridor, everybody with these poppers; the secretaries, anesthetists, nurses, doctors, nurse practitioners, respiratory therapists, just checking all our patients. Most of our patients were finally bending, was completely changed for our life, for our American lives. That day was when we started the pandemic. It was a very rough three weeks, very terrible.
Laura: I can only imagine. Rodney, Victoria speaks about the stress that our health practitioners are feeling, and I'm sure with the long hours you're working and compounded with the potential risk of exposure to the virus that those things are weighing heavy on your mind, how are you coping with that?
Rodney: Yes, I'm keeping myself informed. This is an ongoing thing. We are learning more about this and the more you're informed, the more you are able to handle it better. Also, me and the family are being positive regarding this. We're finding a way to adjust to the new world because as I've said, this is not going away anytime soon, so we just need to learn how to adjust and make the most of it. Of course, we're still doing our due diligence at work and we're still doing our due diligence at home. We're still keeping our social distancing, handwashing, we're trying to wear masks every time just to better protect ourselves.
Laura: Right. How about you, Doreenlove? How are you holding up in keeping sane during these times when so much is happening and you're putting yourself at risk every day?
Doreenlove: I think Rodney said it all. For me, I've had to take my kids to my mom just so that maybe any potential infections that I have don't get to them. It's really not been easy. In addition to what Rodney said, I'll just add that my spiritual life has really been firm. It's been very high within this period. I've seen myself pray more than initially. I've become more prayerful because when I pray, I feel a sense of satisfaction. I feel OK. I feel better. Increased spiritual life in addition to what Rodney said.
Laura: Great. Thank you for sharing that. In the U.S., a lot of states are starting to ease their restrictions. Rodney and Victoria, as nurses on the front lines, what are your feelings about local governments in the U.S. starting to lift these orders? Do you think our health systems are prepared?
Victoria: Actually, I feel that they gave it time with the stay-at-home order to be prepared, but maybe we'll run this back later. Yes, I think that we are prepared.
Laura: How about you, Rodney?
Rodney: I feel we should open up. I feel like the hospitals are more equipped to deal with this. We're getting smarter on how to manage this, and we are getting smarter as well in distributing resources in case of any outbreaks. Also, I feel like there's more equipment out there for us to protect ourselves, there's more respirators. We also instituted some processes in our hospital that we can help out other hospitals just in case they have an outbreak. I think our government and our society should open up, and if ever this thing happens again, I'm pretty sure we're ready for it, and we'll manage it.
Laura: Inspirational message to hear from you guys. Doreenlove, you're a longtime volunteer with our organization and you've filled many different roles and you help beyond just your skills in nursing. Is there anything that you've learned from your experience and volunteerism with Operation Smile that you've been able to apply in your response to this pandemic?
Doreenlove: Yes, I've learned so much from being a volunteer. The first is teamwork. On missions, you work with different teams, multidisciplinary. You are working with doctors, you are working with nurses, even from different countries, even if it's in Ghana, different parts of Ghana. You have to learn how to work in a team. Then also, effective communication, you have to learn how to communicate effectively so that your team members understand what you are saying.
Then, on missions, anything can happen, so you have to think on your feet. It has sharpened my critical thinking abilities. Then, the one thing that has also really helped me is how to manage resources. As a (clinical coordinator), sometimes, you go on a mission – anything can happen on a mission. I remember we went to Ethiopia last 2019, February, our cargo didn't arrive. We had old cargo there. The mission had to go on.
They had flown all of us in-country and there was no cargo, but I was able to manage the resources that we had, and then we had a very good mission. In relating that to the COVID-19 pandemic, we know that there is a shortage of PPEs and all that. Being a (clinical coordinator) and being even a volunteer has made me learn those things. Even at work now, maybe when I see that there is a shortage of PPEs, I know how to ration.
We do three shifts, 6 to 2, 6 to 4, 2 to 8, and then 8 to 8. When you realize that probably, the PPEs are getting low, instead of doing three shifts, you just do two shifts so that you just have the same people wearing PPEs throughout. You don't use more. That's one of the things that being a volunteer has helped me in relation to the COVID-19 pandemic.
Laura: Thank you for that. Victoria, before COVID-19 came into existence, the World Health Organization actually declared 2020, this year, the Year of the Nurse and Midwife. Now, because of this pandemic, that's all the more appropriate, but citizens around the world are seeing how essential the services you as a nurse provide in your community and really to our society as a whole. How does it feel to be recognized as a health hero, and what do these displays of appreciation and recognition mean to you?
Victoria: I really feel very emotional. I'm very happy, I'm very thankful, but at the same time, I feel we're more compromised. It made me better, but sometimes I'm saying, "I'm not a hero. I just do the job that I really like to do, that I love to do.” I do it with more compassion and more love because in this pandemic, teach us that those people started to be alone with no visitors, nobody is going to be next to them. We are bedside nurses face to face with such enemy that we don't know how to get it done.
I feel very appreciated other people recognize how we are at risk to get an infection. Then, I think the hero is where you save the princess to the castle that is in fire. I'm not a hero, but I really do what I like to do, and I can see how I can change the other people lives and I can help the other people be alive also. I'm very grateful for that, and I feel very compromised. I want to work better than I'm doing now with more compassion and more love.
Laura: You can say you're not a hero, but I think the three of you are all very much heroic in putting yourself in the line. It's a dangerous job, and we're so happy to have you guys doing it. To that same point, Victoria spoke about her compassion as one of the things that motivates her. Rodney, could you talk about what's motivating you to keep pushing through and going to work every day during this difficult time?
Rodney: Believe it or not, I'm still enjoying my work. I love taking care of patients, still love being a good resource person to my community. I'm still enjoying learning new things. COVID-19 came really fast and hard on us and we need to learn a lot of new things during this pandemic, but I feel like we're winning. I'm still enjoying this. I still have a lot of love and care to give to my patients, that's why I'm still doing it.
Laura: How about you, Doreenlove? What keeps you motivated and why do you choose to be that first point of contact for the patients that come in?
Doreenlove: I'm a nurse. That's all I know how to. I swore an oath and I have a duty of care to my patients. Just like if it were war, I would expect the military or the soldiers to go. This is my war, so if I don't go, who will go? Do you understand? Society is also looking up to us, me as a nurse, to be at the forefront. That's what motivates me. Then, also my training and experiences has really prepared me, so every time, every day I go to work, I feel I'm giving out my best. Then, this whole COVID-19 pandemic is something new. There is always more to learn, and the more you learn, the more experienced you become. I think it's adding up too, all the experiences that I am getting as a nurse.
Laura: You guys are truly inspirational. Is there anything else that you guys would like to add before we open the floor to audience questions?
Victoria: Yes. Just remind everybody that the virus exists, that the virus is true, that the contacting is true, that we have to take care of each other, that we have to help and support all the heroes and first-line responders. We have to pray that one day, we're going to just get a vaccine or medication, or something that we can treat our patients. Just pray for us. That encourages us to continue to do our job, with more commitment to do our job and take care of our patients.
Rodney: Also, to add to that, I know this is a stressful time for everyone and we need to be more tolerant with each other. Everyone is not having any job. A lot of them are sick. Stay positive. We're getting better, we're managing better, and there will be good times ahead of us. We just need to learn to adjust to the new world out there.
Doreenlove: I also want to add that we as health workers, as we are taking care of our patients, even though there is potential risk to ourselves, we should give our best. We shouldn't forget to stay hydrated, eat well, and then when we are off-duty, we should partake in relaxation activities. Then, we should take care of our mental health because there's so much stress going around. If you need somebody to talk to, talk. Don't just keep everything bottled up, because if we are OK, if we are healthy, that is the only way we can also take care of our patients. That's my little advice to all health workers. Let's take care of ourselves so that we can take care of our patients.
Rodney: That's beautiful, Doreen. I love it.
Doreen: Thank you.
Laura: That's such an important advice because you won't be there to take care of everyone else if you're not taking care of yourselves first. Thank you so much for answering those questions. We have a few more for you. I'm going to kick it off to my colleague, John. There have been a lot of cool inputs, so I'm excited to see what you guys have to say.
Audience Q&A
John: Thanks, Laura. Yes, super excited to enter the question and answer portion of this, and just thank you guys for sharing all of those insights with us, really beautifully said. I just appreciate you guys taking the time. I'll double down on the idea that you are truly heroes, too.
Rodney: Thank you.
John: Okay, let's get into it. Victoria, I think this is a good one for you in your deep experience in the intensive care unit. This is coming from Abreham. What was your first immediate fear when you were joining the COVID-19 team and saw your first patient face-to-face?
Victoria: It was awful. I'm feeling like a panic. I think that the nurses who do bedside care are people really feel – how we feel in front of the patients – I was afraid. I was way more conscious every movement that I do in the patient room. I start to put on my PPE and check every single thing like my N95, my surgical mask, my goggles, my face shield, my surgical cap, my cover shoes, and my gown.
I saw myself in the window before I go into the patient room. I put everything together and I make every single movement more conscious because I feel that I have more risk to get the infection. I have three patients to take care or two patients to take care, everybody is positive, and we don't have treatment, we don't have vaccine, we have nothing. Then, I'm feeling very anxious. I'm feeling panic. I was terrified. I was really terrified. Yes, it's scary because you are face-to-face with somebody who has a virus that we don't know how to treat.
John: Thank you. Kind of the tail end of that question, another one from Abreham, he's asking what was the moment like when your first patient recovered from the condition?
Victoria: Actually, the first admission, this patient was in the bed almost for two weeks. We were thinking that maybe she couldn't make it because she had very long medical history like COPD. A patient with COPD is so difficult to extubate. We can't take any patient with COVID. We cannot. Then, we're waiting and waiting, and we try to wean up from the bed, and almost like three weeks after that, the lady made it and the lady went home. That was one.
We have other that was a miracle. Yesterday, exactly yesterday, last night, the guy who went to the hospital and say hello to us and give us some food for dinner because they are very appreciative of how we've been working. He was one of the survivors also after almost three weeks of bed. He's very emotional, and it's very satisfying that we really did something that kept the patient alive.
John: Thank you.
Rodney: Great job, Victoria.
John: Okay. I think I have a question here for everybody, so if we could go around and each of you can provide this answer for me. We'll start with Rodney. This comes from Anushka, who is one of our wonderful student volunteers from New Jersey … They ask, "After work every day, did you have to quarantine yourself from any family members, and did you have to stay at work?" Rodney?
Rodney: Not quarantine myself. I go to work wearing ordinary clothes, and we put on hospital clothes when we get to the hospital. Then, when we finish our work, we return the hospital uniform and we go back to our normal clothes. Also, me and my wife instituted some things that would help us not bring this virus home because research assesses that the shoes is the big culprit in spreading the virus. I have shoes that just stays in the car.
I have a COVID car, and that's what we use just to go to the hospital. We're very diligent with our handwashing, and we make sure we shower when we get home before we come in contact with our dogs and kids. Those are the things that we do just to prevent us from spreading this disease.
Also, I'm trying to keep myself healthy like rest, because this is a virus. Your body can fight this if your body is healthy. Just eat properly, keep yourself positive, and keep yourself healthy.
John: Yeah, definitely. Doreenlove, how has this experience been for you with your family in terms of quarantine or having to stay apart?
Doreenlove: I think I mentioned this earlier that my husband is also a health care worker. Both of us going to work, we never know what we are bringing home, and my mom is over 60, so we sent her our kids. I have a 3-year-old and a 1-and-a-half-year-old. Both kids are under 4 years, so I sent them to live with my mom so that I can limit my exposure to them. Also, I do basically what Rodney said. Shoes that you take to work, when you get home, keep them in the car. You don't bring them. Of course, before you put them in the car, you have to decontaminate and all of that. Wash your hands.
The first thing you do when you get home is to take a shower. Then, even from friends and family, apart from my kids, I try as much as possible to distance myself from them. That is my own isolation method because I never know what I'm bringing home. Even though in Ghana, we don't have restricted movement, I try not to mingle so much with other friends just because I don't know what potential infections I'm carrying. That is it. That's what I do.
John: Victoria, same question.
Victoria: Yes. As Rodney, we use a scrub at home and in my job. We never use the regular uniform. Then, we just be careful every time that we are at the patient room, we wash our hands 25 seconds, or like three or five minutes. We remove all the clothes over there, and I leave in the hospital, and I take a shower before I come home. When I get home, I go in the garage, I leave everything there, my uniform, my shoes, everything. I go directly to the shower again.
We take care with the mask and social distance with other people. We try and don't go with any meeting or any party. We try just to be isolated because the virus, you don't know where we can get the virus or when you can bring the virus from work.
John: These are tremendous sacrifices that you guys have to make, and we just really appreciate everything you do. I know everyone's had to make sacrifices in some shape or form, but day in and day out, it's just incredible, and we thank you for that. We're getting some really heartfelt messages of thanks coming through our Q&A board right now. Before I kick it into Pat's question, Pat Carter, I want to share that message of thanks with all of you before we get to a very good question coming from her.
She says, "My prayers are with you and your families continuously. Thank you for loving mankind and being completely and totally devoted to your calling as servants to the world. Again, thank you and God bless you and protect you during this time of uncertainty and fear." I just thought that was really beautiful, and thank you, Pat. Pat also asks, "How is the pandemic affecting the work being done for patients needing surgery?" Anybody who want to take a stab at that one?
Doreenlove: Okay. For my hospital, in my country, when our cases started rising, we stopped all elective surgeries. All elective surgeries were stopped, and then we're just doing emergencies. Now, I think most hospitals are opening up and surgeries are being done. We are being more careful. Actually, we are adhering to all the precautionary measures. Surgeries are being opened but not as before, not so much as before. Probably, with time, it would get to pre-COVID-19 state, but now, we are just seeing how it goes. Just little by little. It is better than maybe two weeks ago, three weeks ago.
John: How about in the U.S., Rodney or Victoria, how is this affecting the surgical landscape?
Rodney: My wife being an OR nurse, actually, the same thing happened. They stopped all non-emergent surgeries. OR nurses are redeployed to other areas of the hospital like they were doing screening because there are no elective surgeries. It's opening up now slowly. They're not rushing it in Florida. They're starting to do some elective surgeries. During the height of this, all routine surgeries were canceled.
Victoria: Actually, we have now protocols and procedures in place, or whoever go to elective surgery, they're going to do the test, they're going to test for COVID, and they take all the precaution that we normally have to do, but they already had started slow. They are going to start it slow to see how it's going now.
John: Awesome. Victoria, I have a two-part question coming from two different folks. We have Marcella and Pat. Well, first, they ask, "How many cases of COVID-19 have you seen in your unit that are children?" Then, "Is there a balanced mixture of men or women or is there more from one gender or the other?"
Victoria: Actually, we received just adult people. We don't have a pediatric in the unit that are working. Then, my unit is just 22 beds, but they were opening two more units when we're having a peak within the two first weeks. What we can see is it affects more the male than female. We have more male than female, and also that we can notice also was that the obese people is more affected than the regular and normal-weight people.
Sometimes, we have weird cases where the patient is 95 years old with too many comorbidities and they don't have any symptoms, but we have also 53 years old male with no medical history that couldn't make it. Then, we don't really know what is the pattern of this, but definitely, we saw more in male than female.
John: Awesome. Thank you. I think that will conclude our question-and-answer portion. If there is a question that you asked that wasn't able to be answered, we'll be sure to direct that question to one of our panelists and get you the insight that you need, and we'll follow up via email. Laura.
Laura: Thank you so much, John. Again, thank you so much to the three of you. I know you're so busy and I really appreciate you taking the time to speak with our audiences and to share your expertise but to also share your compassion. The comment that John read aloud perfectly summarizes it. You guys truly are servants to mankind. We really appreciate everything you are doing and the contributions you're making to your communities.
Thanks to all the attendees who joined during this webinar. We'll be sending out a recording of this in the next couple of days. Feel free to share that with any friends. If you'd like to sign up for future COVID Conversations, then you can subscribe to our email list and we'll share information about that. Folks, Doreenlove, Victoria, Rodney, thank you so much.
Latest Stories

A Former Patient, Aymane Now Shares His Story

What is Operation Smile's Nutrition Program?

