
Our promise of improving health and dignity during the COVID-19 pandemic endures. We're helping front-line health workers stay safe, nourished and empowered to better serve their patients by providing life-saving supplies and equipment, as well as remote training to bolster their response. We’re also providing nutritional assistance, hygiene kits and virtual health services to support people and their health needs so they can thrive. If you can, when you can, help us keep our promise to care for children and create hope for tomorrow.
Eager to attend a medical mission in Morocco, volunteer Jen Lin left Seattle in early March ready to change lives – but a little over a week later, she returned home and instantly had to adapt to a new reality.
“In a country of more than 300 million people, I didn't know how quickly it would spread,” Jen said.
As a family medicine physician, Jen works in outpatient urgent care and primary care clinics, delivering much-needed medical care to pediatric and adult patients. But today, she’s being called to bravely serve patients affected by the coronavirus.
Like so many of Operation Smile’s volunteers who are selflessly putting the health and well-being of patients above their own, Jen finds ways to remain hopeful, think innovatively and stay committed amid the pandemic.
“I feel like this is what I was trained to do as a family medicine doctor in urgent care,” Jen said. “We’re trained to be useful in many areas of medicine and to take care of people.”
We recently sat down with Jen to learn what an average day looks like working on the front line in an epicenter of COVID-19 and to hear how her global network of friends in the medical field are joining forces to combat the shortage of necessary resources.
Q: Seattle has some of the highest concentrations of coronavirus cases in the U.S., what challenges and/or limitations have you and your fellow medical professionals faced during the pandemic?
A: “Seattle was the location of the first cases of COVID-19 in the U.S. Initially, our hospitals' protocols were rapidly evolving and no one knew how quickly COVID-19 was spreading or even any specifics about the virus. We all had to be flexible and go where the need was, which, for me, was to a higher risk COVID-19 clinic where I could potentially fall ill or spread it to my family and friends. That was the biggest challenge.
“The other issue was the concern for our limited resource of personal protective equipment (PPE) where we were probably reusing supplies at overly conservative levels early on. But that was based on the information the hospital had at that time.”
Q: Have you experienced any acts of generosity or compassion from other health care professionals in the U.S., or even globally, who are trying to support your hospital?
A: “Absolutely! I have nonmedical acquaintances and friends from China and the U.S. who selflessly very early on in the pandemic used their personal finances to ship N95/KN95 respirators from China to me in the U.S. I received close to 500 masks from them, which I then dispensed to my health care friends at 10 different hospital systems in the Seattle area.
“I wanted to share to as many as I could because we are a team fighting this virus. I'm so touched by their generosity and thoughtfulness in wanting to have these limited resources go directly into the hands of health care workers like me who are on the front lines of this pandemic. Without hesitation, they assisted hundreds of health care workers they've never even met.”
Q: Can you describe your experience with leaving Seattle to attend a March medical mission and how it felt to return home to an almost unrecognizable situation due to COVID-19?
A: “When I left Seattle for Morocco, I had a bit of concern because I think we had nine positive COVID-19 patients, but they were all from the same nursing home 20 minutes from Seattle. I was busy during the mission, so it only really hit me when the president closed borders to multiple European countries two days before we were to come home.
“The majority of us international volunteers were scheduled to transit through those countries. My first shift was the day after I arrived home, so it was a mad rush for me to get up to date on our protocols and guidelines for COVID-19.”
Q: What is the environment like in your hospital currently?
A: “Though the coronavirus started out fast and furious for us here in Seattle, home quarantine has slowed volumes and infections in the primary care and urgent care clinics considerably. We appreciate that people are trying to stay safe at home and come into the clinic and hospital only if absolutely necessary. That also means that we have a high amount of phone calls and online virtual management of our patients. Our hospitals are the ones seeing the critical patients and found the COVID-19 positive patients have a longer duration of hospitalization with prolonged respiratory support. At this time, we have enough hospital beds and ventilators to help our state's patients. But new infections and deaths continue to persist.”

Q: Can you describe your average day once you arrive for work?
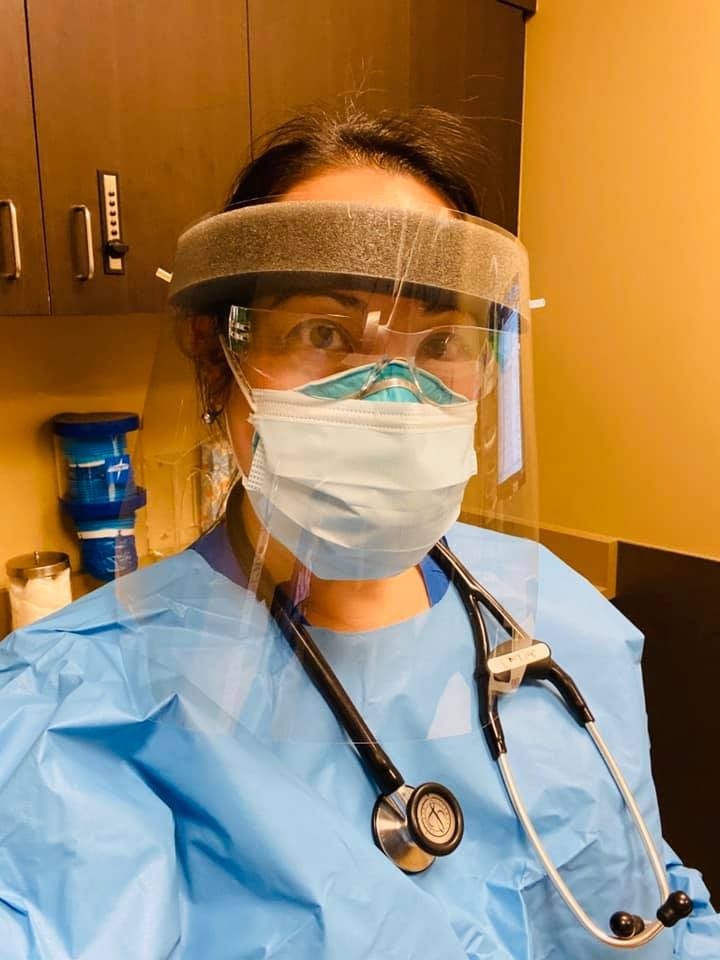
A: “On an average day in urgent care, I do an 8- to 12-hour shift in our acute respiratory COVID-19 urgent care clinic. We spend our time in our PPE. This includes gown on top of our scrubs, a scrub cap, shoe covers, our personal N-95 respirator with a surgical mask on top, goggles, a double set of gloves, and a reusable plastic face shield.
“When we are in this PPE, we often feel hot, claustrophobic, and suffocating, but we are keeping ourselves and our patients as safe as possible. We get one surgical mask per day which we wear all the time in the clinic. I've used my N95 mask for the last three weeks. At this clinic, we see only patients who have any respiratory symptom. which could potentially be due to COVID-19, and we’re the only swab testing on-site for our hospital's clinic network. This helps to relieve other clinics of the potentially contagious patient that could spread illness to other healthy patients or staff, while also effectively conserving the limited PPE. After my shift, I go home, strip at the door and go directly into the shower.”
Q: What have you learned from being involved with Operation Smile that’s helped prepare you for responding to COVID-19?
A: “Flexibility. Our protocols and guidelines for every aspect of this pandemic has been evolving, and protocols, like how we conserve our PPE, sometimes changed mid-day. Just like on an Operation Smile mission, everyone is trying to do their best with what they have. Also Operation Smile has given me the opportunity to make friends all around the world. I was very concerned about my friends in Italy, luckily they are still safe.”
Q: It's a very stressful time in our world right now. How are you doing, personally, with the impact this virus has placed on you as you continue to face this crisis head on?
A: “I feel like this is what I was very well trained to do as a family medicine doctor in primary and urgent care. We are trained to be useful in many areas and to take care of people of all ages with our wide skillset. We manage people who are ill but don't need hospitalization, recognize those who need hospital transfer for critical services to the hospital, and also counsel a large number of other patients who are in emotional distress from illness or fear.
“I'm proud to be a family medicine doctor for this reason. I also have pride to be part of this compassionate multidisciplinary team working on the front lines to give care to those in need. They sacrifice their time and health. Some are separated from their families to keep their children and parents safe and are working extra hours in any department they can due to the high need for trained professionals and staff. This is what we were trained to do. We got this!”

Latest Stories

A Former Patient, Aymane Now Shares His Story
What is Operation Smile's Nutrition Program?

