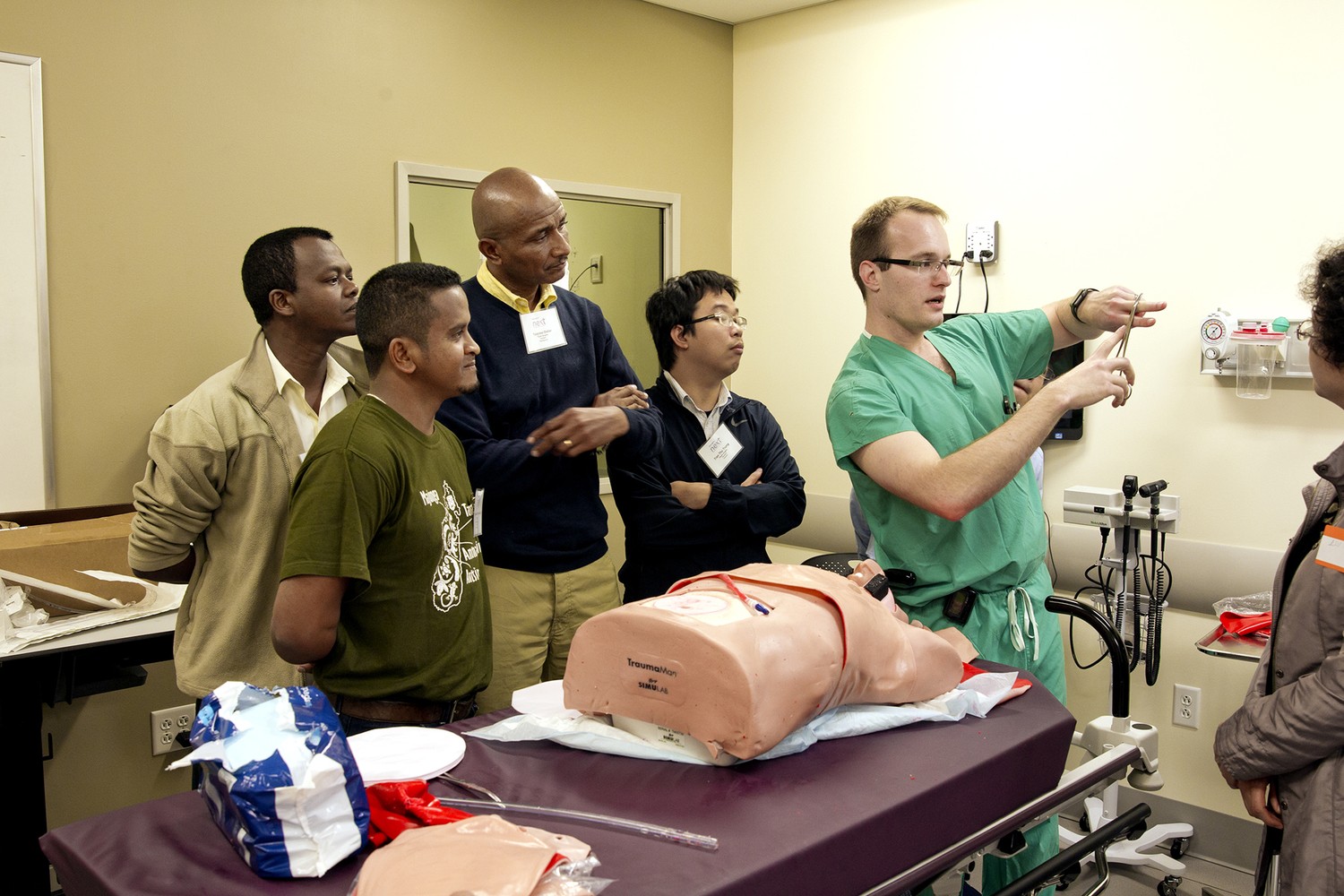
As Dr. Nicholas Bandy made a careful incision on the side of a human torso mannequin, a group of plastic surgery residents from Ecuador, Madagascar, Vietnam and China surrounded the operating table, observing with intense focus as they listened to his instruction.
Dr. Bandy, an Eastern Virginia Medical School (EVMS) resident, emphasized the benefits of the proper technique and warned of the life-threatening consequences of making mistakes on a real-life patient.
For most of the residents, the simulation was their first experience with a tube thoracostomy, the insertion of a chest tube to drain fluid – such as blood resulting from trauma – away from the lungs.
According to the Journal of Thoracic Disease, it’s the most common procedure in thoracic surgery. Yet in some low- and middle-income countries, many surgeons never get the chance to learn these life-saving skills.
That’s why on May 8, 2018, Operation Smile and EVMS hosted a trauma workshop for 40-plus plastic surgery residents and medical volunteers from more than 20 countries as part of the 2018 NEXT Medical Conference in Norfolk, Virginia, U.S.

In addition to two hands-on trauma simulations, EVMS trauma surgeon and educator Dr. Leonard Weireter engaged and challenged the participants in the classroom with lecture- and scenario-based discussions. The workshop followed the Trauma Evaluation and Management (TEAM) training course developed by the American College of Surgeons.
The day before, Operation Smile hosted workshops on pediatric perioperative emergencies at Johns Hopkins Hospital in Baltimore and pediatric anesthesiology at George Washington University Hospital in Washington, D.C.

The majority of these workshops’ participants are fellows of the Regan Resident Leadership Program. Named in honor of its benefactor the Regan family, who exclusively fund the program through their nonprofit Harbourton Foundation, the program provides senior residents in anesthesia, pediatrics and surgery (oral and maxillofacial, plastic and reconstructive) with the unique educational opportunity of attending an Operation Smile medical mission to volunteer under the mentorship of experienced physicians as their assistants.
Its fellows also receive further training and educational opportunities such as attending skills workshops, NEXT conferences and other regional Operation Smile medical conferences within their fellowship year.

One of the Regan fellows taking part of the trauma workshop at EVMS was Ecuadorian plastic surgery resident Dr. David Alvarez. He said the 7-hour course introduced him to skills and knowledge to which he had never been exposed.
“I’ve never inserted a chest tube before, on a mannequin nor a patient,” said David, who has served on 10 Operation Smile medical missions in Ecuador over the past three years. “I also had never performed a (cricothyroidotomy, an incision made to create an airway during certain life-threatening situations including facial trauma), so that’s another experience that I have never had before.
“In Ecuador, it’s not common to take part in a training like this. I think that gaining this experience is really important, because now I can put it into practice at any moment that it’s needed.”

The instructor of the difficult airways simulation, EVMS resident Dr. Nina Cohen, emphasized the importance of teaching her global counterparts life-saving procedures like cricothyroidotomies, which are easier and quicker to perform than tracheotomies and cause fewer potential complications, according to the journal Operative Techniques in Otolaryngology.
“Everything went really great today – I think (EVMS residents and staff) really enjoyed working with people that we normally don’t get to work with,” Dr. Cohen said. “I think everyone really enjoyed the opportunity to be able to go through the steps in a very controlled manner on these really advanced task trainers (mannequins) that we get to work on here. At the end, we even performed intubation on one of (the mannequins), and some of the residents from other countries had never intubated before, so that was a great skill to be able to work on as well.
“It’s a great opportunity anytime you have the chance to give back to something that’s bigger than you are. I’m happy to share our resources here with (the workshop participants) and to have the chance to work through these emergent situations with them.”

Latest Stories

A Former Patient, Aymane Now Shares His Story
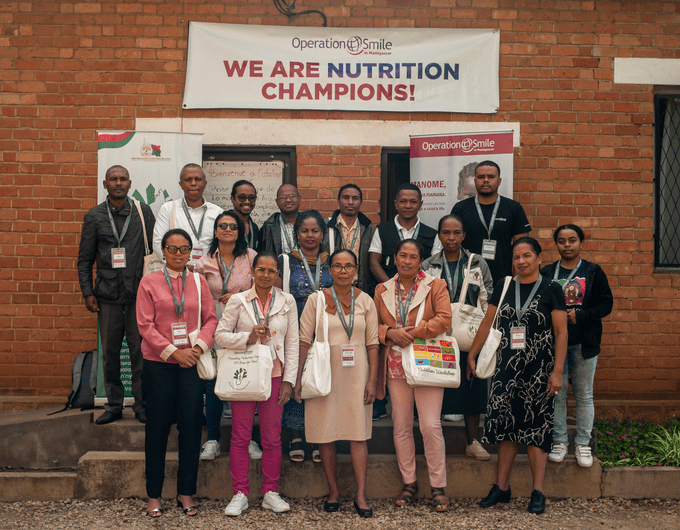
What is Operation Smile's Nutrition Program?

